Causes of Pudendal Neuralgia
Pudendal neuralgia can be caused by various factors, including:
Repetitive Compression: Activities that place constant strain on the pelvic region such as cycling and horseback riding are common risk factors due to the repetitive and prolonged pressure on the pelvic area.
Trauma: Direct injury resulting in acute compression of the pudendal nerve oftentimes due to pressure from surrounding tissues or muscles. Pelvic surgeries such as a hysterectomy or prostate surgery can inadvertently injure the pudendal nerve.
Childbirth: During vaginal childbirth, especially prolonged birth, results in inflammation and injury of the pudendal nerve leading to symptoms seen either immediately after childbirth or later on.
Pathologic: Space occupying lesions such as localized or metastatic tumors including prostate cancer or bladder cancer. Radiation therapy often used to treat pelvic cancers can also lead to local fibrosis which can compress the pudendal nerve.
Symptoms of Pudendal Neuralgia
You may not have any symptoms. However, if you do, the symptoms may gradually develop and worsen over time. The common symptoms of pudendal neuralgia are mild to intense stabbing, burning, or shooting pain that is aggravated while sitting. Other symptoms include:
- Pain that is felt in the buttocks or genital regions
- Numbness or loss of sensation in the genital or pelvic region
- Pain that is aggravated when sitting, and improves when standing or lying down
- Painful sexual intercourse, difficulty achieving an orgasm, erectile dysfunction
Impact of Pudendal Neuralgia
Pudendal neuralgia can lead to several conditions:
- Vulvodynia: A condition characterized by persistent, unexplained pain in the vulvar area. It can be experienced as burning, stinging, rawness, soreness, or irritation.
- Pelvic Floor Dysfunction: A condition where the muscles and ligaments which make up the pelvic floor do not function properly, leading to symptoms such as pelvic pain, urinary or fecal incontinence, and discomfort during sexual activity.
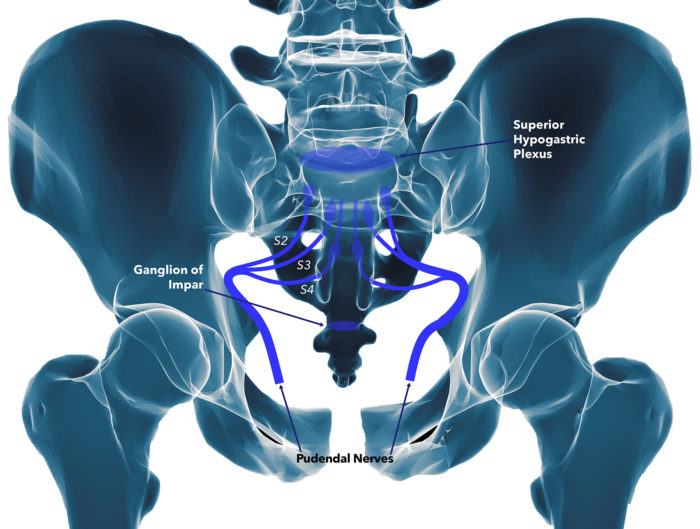
Diagnosis of Pudendal Neuralgia
Diagnosing pudendal neuralgia typically involves:
Medical History: Discussion of symptoms, past medical conditions, and any history of trauma to the pelvic or genital region.
Physical Examination: Assessment of reflexes, muscle strength, and sensation. Vaginal or rectal exams to directly assess the regions supplied by the pudendal nerve.
Diagnostic Imaging: MRI scans to visualize structures surrounding the pudendal nerve. Nerve conduction studies (NCS) in order to assess how well signals travel through nerves.
Diagnostic Nerve Block: Injection of an anesthetic medication, typically lidocaine and a steroid, in order to provide relief to the area that is supplied by the pudendal nerve.
Prognosis of Pudendal Neuralgia
The prognosis of pudendal neuralgia varies widely among individuals. While some respond well to conservative treatments like physical therapy and medication, others may require more invasive interventions such as nerve blocks or surgery for symptom relief.1
Treatment of Pudendal Neuralgia
Treatment options include:
Conservative Treatments: Non-surgical approaches include:
Lifestyle Changes: Avoidance or modification of activities that aggravate the pain seen in pudendal neuralgia; commonly through the use of cushioned seats
Medications: Such as nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants for pain management. Stool softeners if you are having pain with defecation.
Physical Therapy: Exercises to strengthen pelvic and lumbar muscles and improve range of motion.
Nerve Block Procedure: Targeted nerve block procedure to the coccygeal nerve that helps to relieve chronic pain.
Acupuncture or Chiropractic Care: Some patients find relief through alternative therapies.
Surgical Intervention: When conservative measures are ineffective or symptoms worsen, surgery may be considered in extremely rare circumstances:
Partial or Total Coccygectomy: Surgical removal of either part of or complete removal of the coccyx.
Procedure Videos
Pudendal Nerve Block
References
- Pérez-López, F. R., & Hita-Contreras, F. (2014). Management of pudendal neuralgia. Climacteric : the journal of the International Menopause Society, 17(6), 654–656. https://doi.org/10.3109/13697137.2014.912263
- Anand M. Female pelvic pain: Differential diagnosis. In: UpToDate, Connor RF (Ed), Wolters Kluwer. (Accessed on July 20, 2024.)